Junjie Peng1, Tong Tong2, Linghui Xu2, Ying Ding3, Renjie Wang1, Xiaoji Ma1, Sanjun Cai1
1Department of Colorectal Surgery, Fudan University Shanghai Cancer Center, 2Department of Radiology, Fudan University Shanghai Cancer Center, 3Department of Biostatistics, University of Pittsburgh
Objective:The purpose of this study is to develop a
predictive nomogram to improve the diagnostic accuracy and inter-observer
agreement of pre-therapeutic lymph nodes metastases in patients with rectal
cancer, by incorporating pre-therapeutic clinicopathological and MRI imaging
variables. Method: All patients, who underwent preoperative high
resolution MRI scanning and then followed by immediate surgeries for resection
of the primary tumors, were selected in our series. A total of 411 patients
with rectal cancer, locating within 12cm from anal verge, were retrospectively
collected at Fudan University Shanghai Cancer Center between January 2005 and
December 2014. To develop a nomogram, 288 patients were assigned to the
training group; and the other 123 patients were assigned to the validation
group. The variables assessed by high-resolution MRI included primary tumor and
local or regional lymph nodes, including cT category, CRM involvement, tumor
location within the bowel circle, and tumor location related to peritoneal
reflex. The assessment of lymph nodes included the number of detected nodes,
size of the nodes, irregularity of nodes' border and uniformity of signal
intensity within the nodes. All MRI images were read by two independent
observers. Each observer was required to make a diagnosis of N category (N+/N-).
The inter-observer agreement was measured between two observers according to
their original diagnosis of N category. Logistic regression models were
performed to develop a predictive model for the status of lymph node
metastasis. Result: The diagnostic accuracy of MRI-assessed cT
classification was 81.3%; 12.2% of the patients were over-staged and 6.5% of
the patients were under-staged. The diagnostic accuracy of MRI-assessed cN
classification (on the overall data) was 68%; 14.2% of the patients were
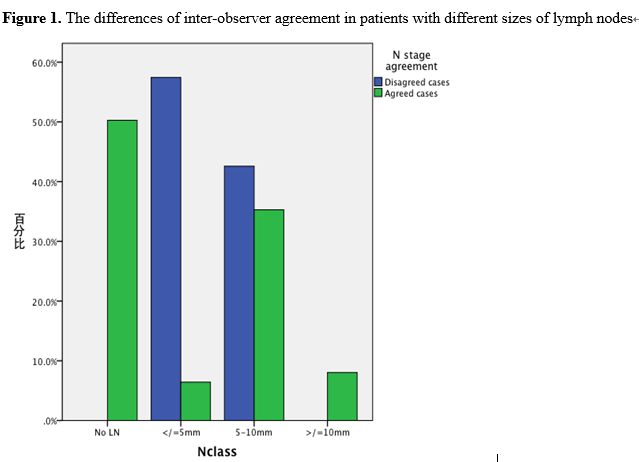
over-staged and 17.8% of the patients were under-staged. We studied the
inter-observer agreement of MRI-assessed cT/cN classification. For cT
classification, the two radiologists disagreed in 3.8% of the patients (11
cases), with a kappa value of 0.905. However, 35.1% of the patients (101 cases)
had disagreed diagnosis for the cN classification by two radiologists, with a
kappa value of 0.295. All the disagreed cases were in the group of detected
lymph nodes with size % of the cases were disagreed in patients with lymph
nodes sizing ≤5mm and 39.4% of the cases were disagreed in patients with
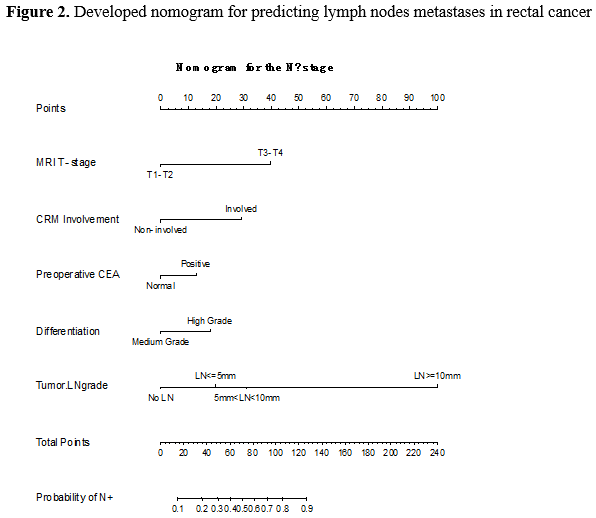
detected lymph nodes sizing>5mm- (Figure 1).A nomogram for lymph node
metastasis was successfully developed, with an AUC of 0.79 in the independent
validation data. The predictors included in the nomogram are cT classification,
CRM involvement, preoperative CEA, tumor grade and MRI-assessed lymph node
classification (Figure 2). Conclusion: By incorporating important
clinicpathological variables and MRI imaging features, our nomogram improved
the diagnostic accuracy and minimized the inter-observer agreement in
diagnosing lymph nodes metastases in rectal cancers.
Key
Words: Rectal cancer Lymph node metastases Nomogram

Copyright © 1998 - 2026 Chinese Society of Clinical Oncology(CSCO). All Rights Reserved
Contact Us
EMAIL:office@csco.org.cn
international@csco.org.cn
Phone:86(10)67726451 (Beijing)
86(25)84547290 (Nanjing)